Understanding the Impact of Digestive Health
Digestive health is foundational to overall well-being, yet conditions like diverticulitis highlight the complexities and vulnerabilities of the gastrointestinal system. Diverticulitis, which involves inflammation or infection of diverticula (small pouches in the colon), often arises due to dietary patterns, lifestyle choices, or genetic predispositions. It can lead to discomfort, serious complications, and, if untreated, long-term health issues.
Modern Lifestyle Impact on Digestive Health
While the condition is more common in older adults, its prevalence in younger populations has increased, attributed to modern diets low in fiber and increasingly sedentary lifestyles. Symptoms such as persistent lower abdominal pain, fever, and irregular bowel movements are disruptive and may signal acute episodes requiring medical attention. Importantly, knowledge about this condition is growing, offering promising strategies for effective management and prevention.
Empowering Through Informed Health Choices
In this article, we explore how informed dietary changes, holistic lifestyle adjustments, and evidence-based therapeutic interventions can empower individuals to reduce the risks and challenges associated with diverticulitis. By integrating these approaches, patients can reclaim control over their digestive health.
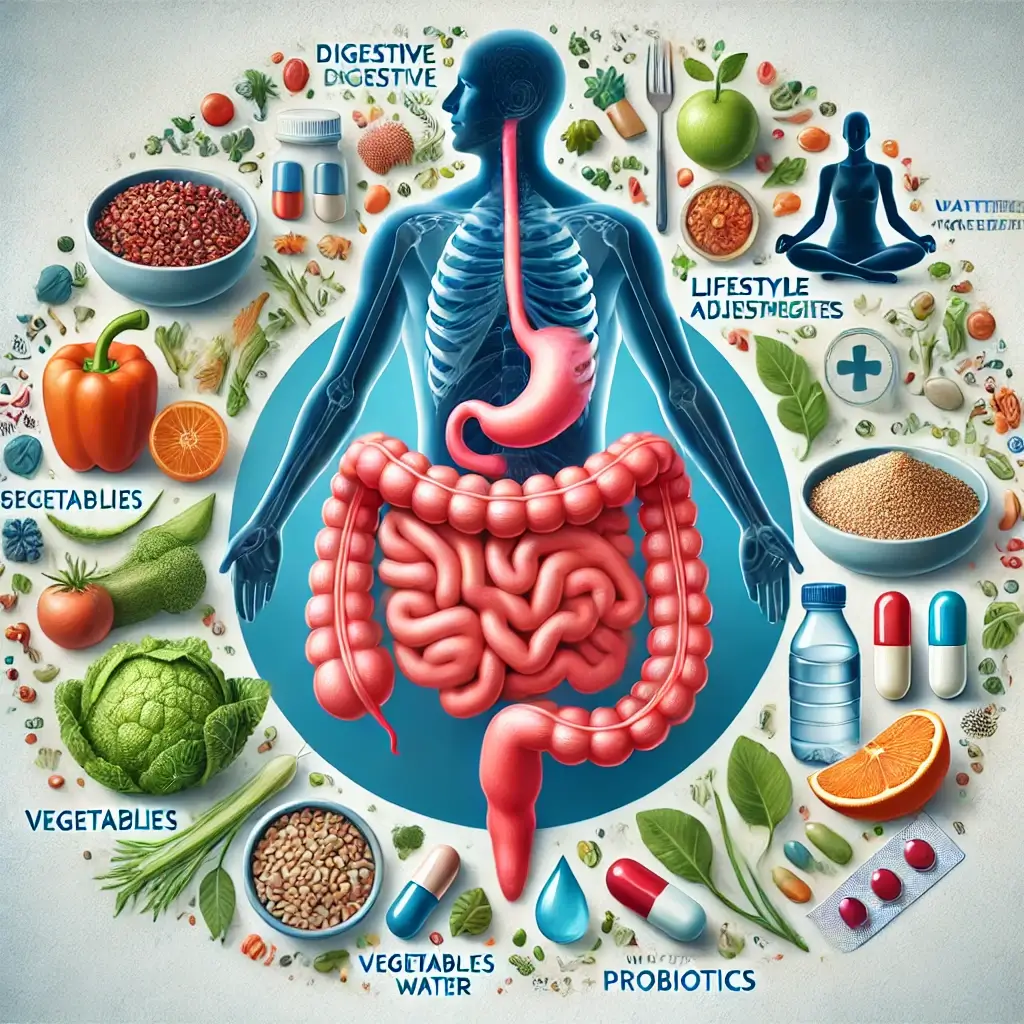
Essential Management Strategies
A multifaceted plan that incorporates diet, lifestyle, and medical treatment is essential for managing diverticulitis effectively. Below, we delve into these strategies supported by scientific evidence.
The Critical Role of Dietary Fiber
The Fiber Factor Fiber plays a critical role in preventing diverticulitis and managing symptoms. A high-fiber diet is essential for long-term prevention, as it helps reduce pressure on the colon by promoting soft, regular stools. However, during acute episodes, a low-fiber diet is recommended to minimize irritation. According to research in The American Journal of Gastroenterology, increasing fiber intake post-flare-up decreases recurrence rates significantly (Peery et al., 2018).
Nutritional Components for Digestive Health
Key high-fiber foods include: Vegetables: Artichokes, carrots, and spinach. Legumes: Lentils, black beans, and chickpeas. Whole Grains: Oats, barley, and quinoa. Hydration and Digestive Health Staying hydrated is critical when increasing dietary fiber. Insufficient fluid intake can lead to constipation, aggravating symptoms. Aim for at least 8-10 glasses of water per day to maintain optimal gut function.
Protein Selection for Gut Health
Diets high in red and processed meats have been associated with an elevated risk of diverticulitis. Replacing these with plant-based proteins, fish, or poultry can help reduce inflammation and improve overall gut health (Gut, 2019).
Exercise and Prevention Strategies
Regular physical activity significantly reduces the risk of developing diverticulitis. Exercise improves gastrointestinal motility, reducing constipation and the pressure on the colon that can lead to diverticula formation. A large-scale study published in Medicine and Science in Sports and Exercise found that individuals engaging in regular moderate exercise, such as brisk walking or cycling, had a 25% lower risk of diverticulitis.
Mental Health and Digestive Wellness
Stress is a major contributor to gastrointestinal disorders, including diverticulitis. Chronic stress disrupts the gut-brain axis, leading to inflammation and irregular bowel habits. Techniques such as mindfulness meditation, yoga, or even simple breathing exercises can help regulate stress and promote better digestive health.
Impact of Smoking on Gut Health
Smoking has been linked to a weakened colon lining and increased risk of inflammation. Quitting smoking not only enhances gut health but also reduces the likelihood of developing complications associated with diverticulitis.
Medical Treatment Options
In cases of acute diverticulitis, antibiotics remain a mainstay treatment, especially when infection is present. Common regimens include amoxicillin-clavulanate or ciprofloxacin combined with metronidazole.
Role of Probiotics in Treatment
Probiotics have gained attention for their role in maintaining gut microbiota balance and reducing inflammation. Studies in World Journal of Gastroenterology suggest that specific strains, such as Lactobacillus acidophilus and Bifidobacterium bifidum, can aid in preventing recurrent diverticulitis.
Surgical Interventions
For individuals experiencing recurrent or severe complications, surgical interventions like colon resection may be necessary. This is generally reserved for patients who have not responded to less invasive treatments.
Comprehensive Management Approach
Diverticulitis is a challenging condition, but with informed choices and a proactive approach, it can be effectively managed. Adopting a high-fiber diet, staying hydrated, engaging in regular physical activity, and managing stress are foundational steps toward better digestive health. Additionally, medical interventions, including antibiotics and probiotics, provide robust options for managing acute episodes and preventing recurrence.
Professional Guidance and Long-term Success
Ultimately, collaboration with healthcare professionals is key to creating a personalized management plan that addresses individual needs. By embracing these strategies, individuals can not only mitigate the symptoms of diverticulitis but also significantly enhance their overall health and quality of life.
Scientific References
Peery, A. F., et al. (2018). High dietary fiber intake and its role in reducing diverticulitis recurrence. The American Journal of Gastroenterology, 113(7), 1036-1044.
Gut. (2019). Red meat and processed meat consumption linked to diverticular disease: A systematic review and meta-analysis. Gut, 68(5), 844-855.
Medicine and Science in Sports and Exercise. (2020). The impact of physical activity on diverticular disease risk. Med Sci Sports Exerc, 52(4), 745-752.
World Journal of Gastroenterology. (2020). Probiotics in diverticular disease management. World J Gastroenterol, 26(25), 3648-3658.