The Role of Mycobiome: Yeast and Fungi in Your Gut Ecosystem
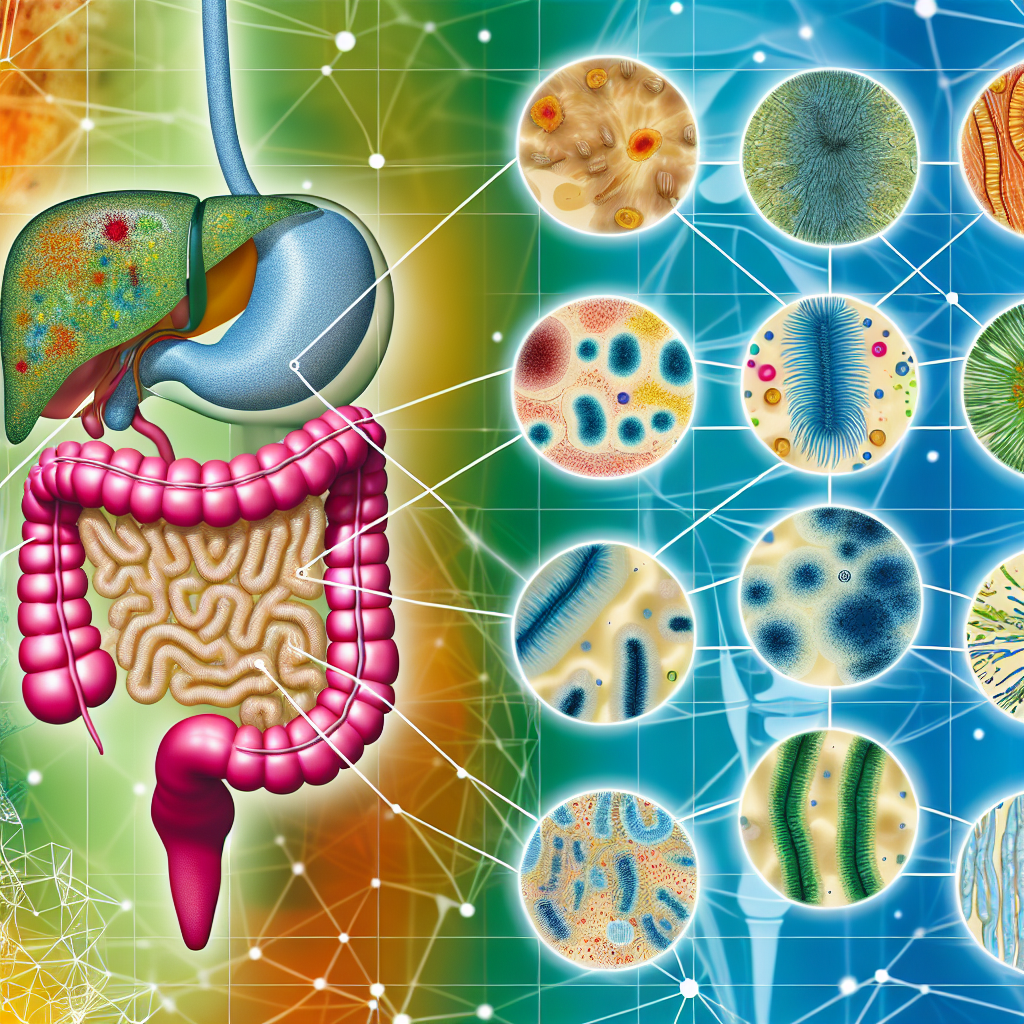
Over the past decade, the conversation surrounding gut health has shifted from a narrow focus on bacteria to a broader exploration of the entire microbial ecosystem residing in the digestive tract. While much of the attention has traditionally been on beneficial bacteria like Lactobacillus and Bifidobacterium, recent research has begun to illuminate another vital component of the gut microbiome: the fungal community known as the mycobiome.
The mycobiome is the collection of fungi, including yeasts and molds, that naturally inhabit the gastrointestinal tract. Although fungi comprise a smaller percentage of the gut microbiota compared to bacteria, they play a disproportionately significant role in maintaining gut homeostasis. Fungi not only interact with other microbes in the gut but also with the host immune system, shaping inflammatory responses, digestion, and even nutrient absorption.
One of the most well-known gut fungi is Candida, particularly Candida albicans. While this yeast is normally kept in balance by other microbes, dietary imbalances, chronic stress, antibiotics, or a weakened immune system can trigger overgrowth, leading to candidiasis and a cascade of gastrointestinal disturbances such as bloating, gas, fatigue, and irregular bowel movements.
Increasingly, natural health advocates and integrative medicine practitioners are looking at ways to support the mycobiome through dietary choices, herbs, and lifestyle modifications. The goal is to create a gut environment that supports not only bacterial but also fungal equilibrium — reducing the likelihood of harmful overgrowth while enhancing the beneficial roles fungi can play in immunity and nutrient metabolism.
The study of the mycobiome is still in its early stages, yet the growing body of clinical and preclinical research indicates that a balanced fungal population could be just as crucial to gut health as a balanced bacterial one. Understanding these interactions opens up new avenues for natural therapies, including antifungal herbs, fermented foods, and immune-modulating supplements that may enhance gut health holistically.
As awareness of the gut’s fungal residents grows, more individuals are seeking natural strategies to support and optimize their entire gut microbiome — bacteria, fungi, and beyond — for better digestion, immunity, and overall vitality.
Fungi in the Gut: New Scientific Insights into the Mycobiome
The scientific study of the mycobiome is revealing fascinating insights into how fungi contribute to gastrointestinal health and disease. While research is still evolving, several promising studies have emerged that deepen our understanding of this critical yet overlooked aspect of the gut ecosystem.
A landmark study published in 2017 in the journal Gut examined the interplay of gut bacteria and fungi in individuals with Crohn’s disease. Researchers found significant differences in fungal composition between healthy and affected individuals, particularly higher levels of Candida tropicalis in those with Crohn’s. This yeast appeared to co-aggregate with certain bacterial species to form aggressive biofilms that may contribute to inflammation (Sokol et al., 2017). This study highlights the potential pathogenic role fungi can play when out of balance and how fungal-bacterial synergy may underlie some chronic digestive issues.
Another important piece of research, published in mBio by the American Society for Microbiology in 2020, explored how antifungal treatments could alter the gut mycobiome. Interestingly, antifungal medications led to compensatory changes in the bacterial population, suggesting a deeply interconnected relationship between bacterial and fungal communities. Disrupting one side of the gut ecology invariably affects the other, reinforcing the importance of a holistic approach (Wheeler et al., 2020).
Natural antimicrobials have also been examined for their ability to modulate fungal populations. Studies on garlic (Allium sativum), for instance, have demonstrated its potent antifungal properties, particularly against Candida albicans. Incorporating garlic into the diet or supplement regimen may help manage fungal balance in the gut without the broad-spectrum disruptions caused by pharmaceutical antifungals (Ankri & Mirelman, 1999).
Probiotics too have been shown to influence the mycobiome positively. A study in Beneficial Microbes found that oral supplementation with Saccharomyces boulardii, a beneficial yeast, could inhibit the growth of pathogenic Candida and modulate immune responses in the gut. This naturally derived probiotic can be especially useful for individuals dealing with recurrent yeast imbalances or gut dysbiosis (Czerucka et al., 2007).
Finally, diet remains one of the most powerful tools for shaping the microbial and fungal landscape of the gut. High-sugar and processed diets tend to feed opportunistic yeasts, whereas fiber-rich, plant-focused eating patterns can support microbial diversity and suppress fungal overgrowth. Herbs like oregano oil, pau d’arco, and berberine have also gained popularity for their natural antifungal properties and ability to support a healthy microbial environment.
Together, these studies emphasize a growing recognition in medical and scientific communities of the essential role fungi play in the gut. They also reinforce the need for natural, targeted strategies that promote balance rather than indiscriminate eradication.
Taking Action: Natural Ways to Support a Healthy Mycobiome
– Incorporate antifungal foods and herbs: Garlic, oregano oil, and berberine can naturally combat fungal overgrowth.
– Use targeted probiotics: Try supplementing with Saccharomyces boulardii to help balance gut yeast levels.
– Reduce sugar intake: Lowering added sugars helps starve problematic yeasts like Candida.
– Eat fiber-rich foods: Support overall gut diversity with prebiotic plant fibers to nourish good microbes.
– Support immune health: A strong immune system keeps both fungal and bacterial populations in check.
Conclusion: Embracing the Mycobiome in Your Wellness Journey
The mycobiome represents an exciting frontier in gut health, emphasizing the critical role fungi and yeasts play within our digestive ecosystem. As we deepen our understanding of the mycobiome, it becomes clear that a healthy gut requires harmony not just among bacteria, but also within the fungal population residing in the gastrointestinal tract.
Through informed dietary choices, herbal remedies, and probiotic use, individuals can naturally support a balanced mycobiome — potentially easing digestive issues, improving immunity, and boosting overall wellness. For those embracing holistic gut health, understanding and nurturing the gut’s fungal residents could be the missing piece in achieving lasting digestive harmony.
References
– Sokol H, Leducq V, Aschard H, et al. Fungal microbiota dysbiosis in IBD. Gut. 2017;66(6):1039–1048. Link
– Wheeler ML, Limon JJ, Bar AS, et al. Immunological consequences of intestinal fungal dysbiosis. mBio. 2020;11(3):e03395-19. Link
– Ankri S, Mirelman D. Antimicrobial properties of allicin from garlic. Microbes and Infection. 1999;1(2):125–129. Link
– Czerucka D, Piche T, Rampal P. Review article: yeast as probiotics – Saccharomyces boulardii. Alimentary Pharmacology and Therapeutics. 2007;26(6):767–778. Link
Concise Summary:
The gut microbiome consists of not only beneficial bacteria but also a community of fungi known as the mycobiome. Recent research has highlighted the critical role of the mycobiome in maintaining gut health and immune function. Natural strategies to support a balanced mycobiome, such as incorporating antifungal herbs, probiotics, and a fiber-rich diet, can help address digestive issues and promote overall wellness.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com