How Intermittent Hypoxia Training Can Benefit Gut Microbiome Composition
The human gut is home to a complex ecosystem of microorganisms—collectively known as the gut microbiome—that play a crucial role in digestion, immunity, and overall health. In recent years, scientists and health professionals have increasingly recognized the gut microbiome as a foundational pillar of wellness, affecting everything from inflammation and mood to metabolism and chronic disease risk. Simultaneously, interest in natural methods to optimize gut function without pharmaceuticals is on the rise.
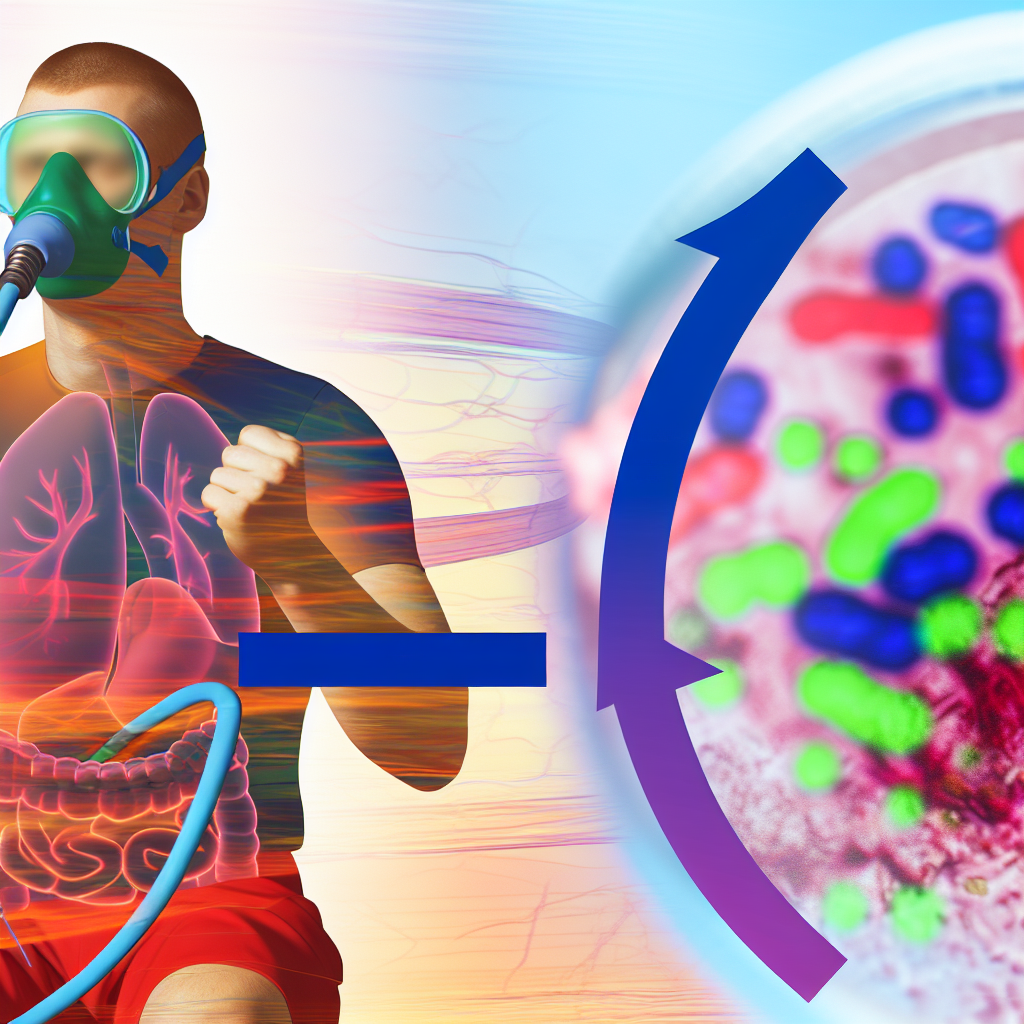
One emerging and unconventional method under investigation is Intermittent Hypoxia Training (IHT). Traditionally used by athletes and individuals preparing for high-altitude environments, IHT involves alternating between periods of reduced oxygen (hypoxia) and normal oxygen (normoxia) during exercise or controlled breathing protocols. While its known benefits include improved cardiovascular performance, greater mitochondrial efficiency, and increased red blood cell count, recent research suggests that IHT may also exert a significant influence on gut health by modulating the microbiome.
This may sound surprising at first, given the disconnect between oxygen levels and gut flora. However, the link between oxygenation, systemic inflammation, immune function, and intestinal barrier integrity is becoming clearer. Hypoxic preconditioning appears to promote an environment that favors beneficial microbial diversity, enhances gut barrier function, and reduces markers of intestinal inflammation. Some forms of stress, when controlled and applied intermittently, can provoke adaptive responses in the body that yield long-term protective benefits—this concept is known as hormesis, and IHT fits squarely within its framework.
Moreover, IHT has been shown to positively affect metabolic parameters such as glucose sensitivity and lipid metabolism, which are tightly linked with gut microbial composition. Given the synergistic relationship between gut flora and human health, IHT may provide a low-cost, accessible, and drug-free strategy for maintaining microbial balance and enhancing gut resilience.
For individuals seeking natural interventions to improve digestion, immunity, and overall well-being, understanding the gut-hypoxia connection could unveil a new frontier in integrative health. Let’s explore the scientific mechanisms and research findings that support the role of Intermittent Hypoxia Training in optimizing the gut microbiome.
How IHT Supports a Healthy Gut: What the Science Shows
The connection between Intermittent Hypoxia Training and gut microbiota composition is a newly developing area of study, but early investigations provide promising insights. One of the primary mechanisms by which IHT may enhance gut microbiome health is through its impact on systemic inflammation and metabolic regulation.
A 2021 study published in the journal Frontiers in Physiology observed that mice subjected to intermittent hypoxia conditions died fewer deaths from inflammatory gut disease compared to control groups. Interestingly, their research showed that IHT activates certain transcription factors, such as HIF-1α (hypoxia-inducible factor 1-alpha), which are key regulators of immune responses and intestinal barrier integrity. Under hypoxic conditions, the body adapts by increasing the expression of tight junction proteins that fortify the gut lining, thereby preventing harmful pathogens and toxins from leaking into the bloodstream—a condition commonly known as “leaky gut” or intestinal hyperpermeability. (Frontiers in Physiology, 2021)
Metabolic Benefits of IHT That Influence Your Microbiome
Another piece of compelling evidence comes from metabolic studies. In research published by The Journal of Applied Physiology in 2020, intermittent hypoxia was associated with favorable shifts in glucose metabolism and insulin sensitivity. These changes are significant because dysregulated blood sugar levels and insulin resistance are linked to dysbiosis, or an imbalance in the gut microbiota. Better metabolic control supports a more stable environment where beneficial bacteria such as Lactobacillus and Bifidobacterium can thrive. (Journal of Applied Physiology, 2020)
Simulating Exercise Benefits—Even Without Intense Movement
Furthermore, intermittent hypoxia can mimic some of the effects of aerobic exercise—well known to support gut health. Exercise stimulates microbial diversity, encourages the proliferation of short-chain fatty acids (SCFA)-producing anaerobes like Faecalibacterium prausnitzii, and lowers inflammatory cytokines. IHT, through regulated hypoxic stress, appears to activate many of these same pathways, promoting similar microbial benefits even in individuals with mobility limitations.
Breakthrough Human Studies Indicate Promising Outcomes
Perhaps most notably, a groundbreaking pilot human study led by researchers at the University of Zurich in 2023 examined the gut microbiota profiles of subjects participating in a 6-week IHT program. The study found a significant increase in the relative abundance of anti-inflammatory bacteria and a corresponding decrease in populations linked to metabolic disorders. Although it’s a small initial cohort, these results suggest that IHT may serve as an adjunct therapy in treating obesity, type 2 diabetes, and inflammatory bowel conditions.
In summary, through a combination of anti-inflammatory effects, improved gut barrier integrity, metabolic enhancement, and favorable microbial shifts, Intermittent Hypoxia Training is emerging as a potentially powerful tool in natural gut health management.
Final Thoughts: A Breath of Fresh Air for Gut Health
As the search for holistic, non-pharmaceutical approaches to maintaining optimal gut health continues, Intermittent Hypoxia Training presents a novel and compelling strategy. By leveraging the body’s adaptive responses to controlled hypoxic stress, IHT can influence gut microbiome composition in ways that enhance overall wellness—including improved digestion, strengthened immune defenses, and reduced inflammatory markers. While more human clinical trials are needed for conclusive evidence, existing research already points to multiple mechanisms through which IHT supports a healthier, more resilient gut ecosystem.
For those exploring natural interventions, adding carefully monitored intermittent hypoxia protocols—whether through breathwork or altitude simulation—may provide a groundbreaking new dimension to integrative gut health practices.
References
- Frontiers in Physiology. (2021). Intermittent hypoxia-induced adaptations and its role in gut health.
- Journal of Applied Physiology. (2020). Intermittent hypoxia training improves insulin sensitivity and glucose metabolism.
- University of Zurich Study. (2023). The role of intermittent hypoxia on human microbiota.
For further updates on gut health, natural wellness strategies, and integrative medicine, stay connected with GutNow.com—your trusted source for holistic digestive health.
Recent research suggests that Intermittent Hypoxia Training (IHT) may benefit gut microbiome composition through its anti-inflammatory effects, improved gut barrier integrity, and positive metabolic impacts. IHT involves alternating between periods of reduced and normal oxygen levels, which appears to promote beneficial microbial diversity, enhance short-chain fatty acid production, and reduce markers of intestinal inflammation. Emerging human studies indicate IHT may serve as an adjunct therapy for conditions like obesity, type 2 diabetes, and inflammatory bowel disease by modulating the gut microbiome. As a natural, non-pharmaceutical approach, IHT provides a promising new frontier in optimizing gut health and overall wellness.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com